
Deworming and Elimination
Schistosomiasis and STH are neglected tropical diseases (NTDs) that thrive in underdeveloped areas where access to clean water and sanitation is limited. More than one billion people are infected with these parasitic infections, which can exacerbate social and economic challenges and trap entire communities in cycles of poverty.
Political will to control and eliminate NTDs has increased in recent years. The Sustainable Development Goals call for an end to the epidemic of NTDs by 2030. The 2012 London Declaration on NTDs brought together pharmaceutical companies, donors, endemic countries and non-government organisations to support the control, elimination and eradication of ten NTDs by 2020.
As a result, national deworming programmes have scaled up mass drug administration (MDA) campaigns, resulting in significant progress to reduce disease prevalence. Although a positive step, programmes have almost exclusively relied on MDA targeting school aged children, who are disproportionately affected by the diseases. But can elimination be achieved and sustained without treating adults or improving environmental conditions?
Recent mathematical modelling by researchers at the London Centre for NTD Research (LCNTDR) suggests that transmission of STH and schistosomiasis can be broken in certain areas using comprehensive cross-sectoral and inter-disciplinary approaches.
The Geshiyaro Project
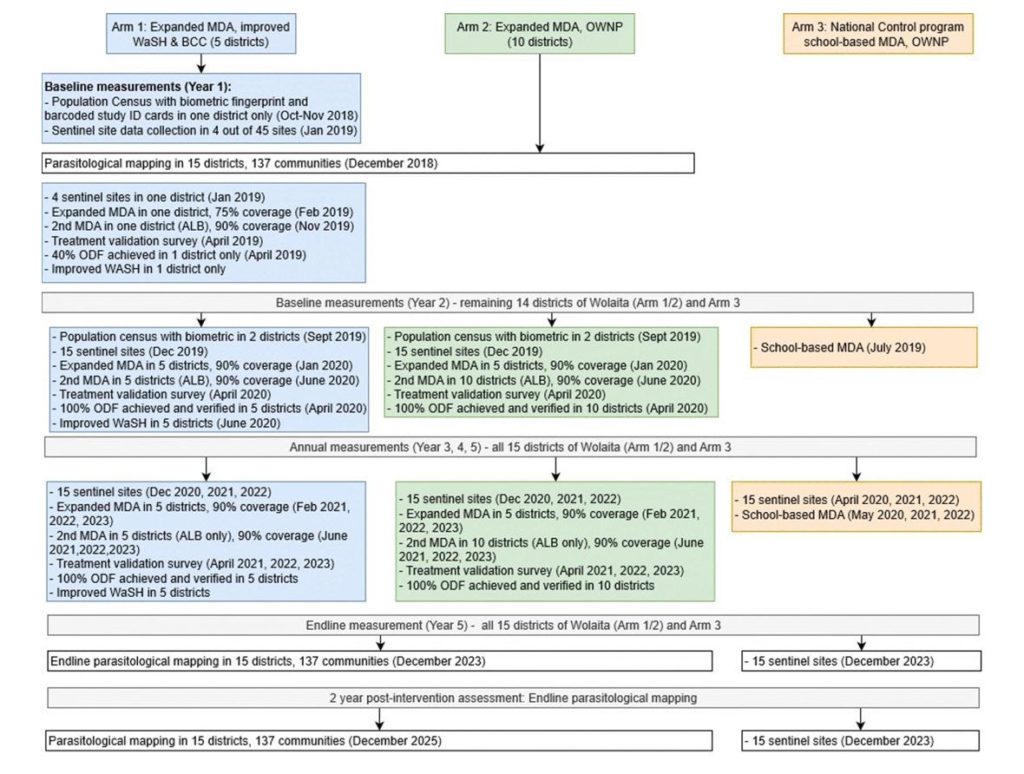
The Geshiyaro Project will research optimal programming and assess three different strategies for delivering drugs and WASH interventions for schistosomiasis and STH control:
-
Expanded MDA and improved WASH: Arm one expands drug distribution beyond school aged children and treats entire communities that are endemic for schistosomiasis and STH. In addition, communities in this arm will receive improved access to WASH interventions, including new wells and public taps providing clean water, latrines for improved sanitation, behaviour change communication, and health education to complement the improved infrastructure.
-
Expanded MDA: Arm two also expands drug distribution beyond school aged children and treats entire communities. However, there will be no further efforts to increase WASH activities beyond Ethiopia’s existing One WASH National Programme.
- Annual school-based MDA: The third arm of the project maintains the status quo and will provide regular MDA to school aged children, with no improvements to the existing One WASH National Programme in Ethiopia.
The study will evaluate results from each arm after four rounds of MDA and will contribute to the design of future of STH and schistosomiasis programmes by providing evidence about the costs and effectiveness of each set of interventions.
Biometric Fingerprint Tech
To improve data collection and our understanding of compliance over multiple years and rounds of MDA, the study incorporates biometric fingerprint technology to identify and track an estimated 750,000 participants in 5 study districts. This innovative approach is expected to help researchers monitor treatment progress over the course of the project, assess compliance and identify systematic non-compliers, as well as overcome challenges associated with usual approaches, such as lost ID cards.

The WASH element
Despite the implicit connection, empirical evidence linking the benefits of WASH activities and associated reductions in NTDs is limited. The Geshiyaro Project aims to expand the evidence base around WASH and NTD integration and the costs involved, which has the potential to greatly improve coordination between the WASH and health sectors.
Developing a scalable model of interventions for the interruption of STH and schistosomiasis is essential if countries are to achieve targets set in the London Declaration on NTDs and the Sustainable Development Goals. Improving access to WASH has the potential to eliminate the need for long-term repeated MDA and improve the health and quality of life of some of the world’s poorest and most marginalised communities, making it an urgent priority for all stakeholders working towards a world free of NTDs.
The Geshiyaro project is an international collaboration between the London Centre for Neglected Tropical Disease Research, World Vision Ethiopia, the Ethiopian Public Health Institute (EPHI) and Ethiopia’s Federal Ministry of Health, with funding from the Children Investment Fund Foundation.

Comments