In recent weeks, reports and discussions on the prevalence and health effects of obesity in the UK and wider afield have been uppermost in the news. An individual is considered obese when their Body Mass Index (BMI), a measurement obtained by dividing a person’s weight by the square of the person’s height, exceeds 30 kg/m2. A better measure of excess fat is waist circumference and, generally, men with a waist circumference of 94cm or more and women with a waist circumference of >80cm are more likely to develop obesity-related health problems.
Obesity is considered to lead to number of serious and potentially life-threatening conditions, such as: type 2 diabetes, coronary heart disease, some types of cancer, such as breast cancer and bowel cancer plus stroke. It is also known to negatively affect quality of life and has been linked to psychological problems, such as low self-esteem and depression. Other day-to-day problems include: breathlessness, increased sweating, snoring, difficulty doing physical activity and joint and back pain amongst others, as described on the NHS choices obesity section and on the associated Complications page.
Dame Sally Davies, Chief Medical Officer for England, recently authored a commentary in the Daily Telegraph entitled: ‘Obesity is an issue that nobody can afford to ignore’ where she discusses potential threats to health, as well as measures being taken to encourage healthy eating. ‘Pilots have shown that kids who receive a free school meal are eating more vegetables and fewer crisps at lunchtime. ‘ This dovetails with the plans to include cooking in the national curriculum which aims to educate children ‘making it easier to learn about healthy eating and a good, balanced diet.’
She also describes the current activities on the part of the food and drinks industry where many key businesses have pledged to reduce calories in their meals and drinks formulations.
She concludes:
‘But I am afraid there is no magic bullet. It is going to take continued effort from all of us in Government, local communities, industry and individuals. Each and every one of us has to play our part if we want to be the first country in the world to reverse this trend [of growing obesity]’.
An obesity paradox?
However, not all researchers are convinced that being overweight or obese is completely detrimental to our health, referring to an ‘obesity paradox’. A new book on this subject entitled ‘The Obesity Paradox: When Thinner Means Sicker and Heavier Means Healthier’ claims that the individuals with certain chronic diseases who lived the longest were the fattest, in some studies. Author Carl Lavie explains that some types of fat are healthier than others: essential fat versus storage fat. The former is held in small amounts in muscle, bone marrow, around organs and in the central nervous system. In men this accounts for around 3% body weight and in women rises to 12%.
However, some researchers have questioned the validity of these conclusions, instead suggesting that the paradox is the result of biases in the studies selected . Writing in the journal Epidemiology, Hailey Banack and Jay Kaufman, biostatisticians from University of Montreal argue:
‘Several prospective studies have reported a J-shaped relationship between obesity and mortality, suggesting increased risk of death in the lowest and highest body mass index (BMI) groups in men and women of all ages, races, and ethnicities‘ including this article by Adams KF, et al. ‘Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763–778’ .
‘Although obesity is associated with a higher overall mortality risk in the general population, some authors have interpreted these patterns to suggest that obesity confers a survival advantage in surviving clinical subpopulations’ One example is the study by McAuley and Blair from 2011.
Banack and Kaufmann propose that the paradox ‘is simply the result of collider stratification, a source of selection bias that is common in epidemiologic research.’
New developments in obesity studies
BioMed Central publishes extensively on the subject of obesity both in the specific medical journal: BMC Obesity,and also in other journals where obesity-relevant research is published, such as, BMC Immunology, BMC Cardiovascular Disorders or the Independent journal in the BMC stable: Journal of Eating Disorders.
In this blog we wanted to highlight an article which has recently been published in BMC Immunology: IL-33 is negatively associated with the BMI and confers a protective lipid/metabolic profile in non-diabetic but not diabetic subjects
This study examined serum levels of a newly identified member of the interleukin family-1 – IL-33 – in lean, overweight and obese diabetic or non-diabetic individuals and correlated these with clinical and metabolic measures.
The authors explain that recent studies have ‘demonstrated a protective role for IL-33 against
obesity-associated inflammation, atherosclerosis and metabolic abnormalities.’
‘IL-33 promotes the production of T helper type 2 (Th2) cytokines, polarizes macrophages towards a protective alternatively activated phenotype, reduces lipid storage and decreases the expression of genes associated with lipid metabolism and adipogenesis.’
The authors objective was to determine the level of serum IL-33 in non-diabetic and diabetic subjects, and to correlate these levels with BMI and body weight (clinical ) and serum lipids and glycated haemoglobin (HbA1c) (metabolic) parameters.
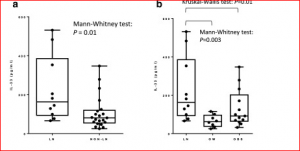
However, a large proportion of the subjects had IL-33 levels that fell below that detectable by the kit used (<23.44 pg/ml). Restricting their analysis to 32% (46) of subjects, the report that the non-lean subjects in their study exhibited significantly lower levels of IL-33 compared to the lean controls, with IL-33 negatively correlated with the BMI and body weight in lean and overweight, but not obese (non-diabetic and diabetic), subjects (see figure above).
In light of these findings, they propose that IL-33 may be involved in mechanisms which are protective against insulin resistance, with IL-33 positively associated with protective lipid profiles, and negatively correlated with HbA1c in non-diabetic subjects.
The authors interpret their data to suggest that reduced levels of IL-33 may put certain individuals at increased risk of developing insulin resistance and atherosclerosis, and may serve as a novel marker to predict those who may be at increased risk of developing atherosclerosis. However, they also point out that the small number of subjects studied may have impacted their ability to reach definitive conclusions ‘and further mechanistic studies are warranted.’
The obesity debate will continue for some considerable time and increasingly extensive resources will be required in the health services to counter and medicate this condition. However, continuing research on the subject will allow researchers, the medical profession and individuals to understand better the protective mechanisms our bodies have against obesity.
Comments